A root canal specialist plays a vital role in preserving natural teeth affected by infection, trauma, or deep decay. When discomfort, sensitivity, or inflammation originates from within the tooth, specialized care becomes essential to prevent complications and maintain oral function. Understanding the role of a root canal specialist helps individuals make informed decisions about dental health and reduces anxiety often associated with endodontic procedures.
This article provides a detailed, educational overview of what a root canal specialist does, the problems they address, why these issues occur, and how early awareness can protect long-term oral health.
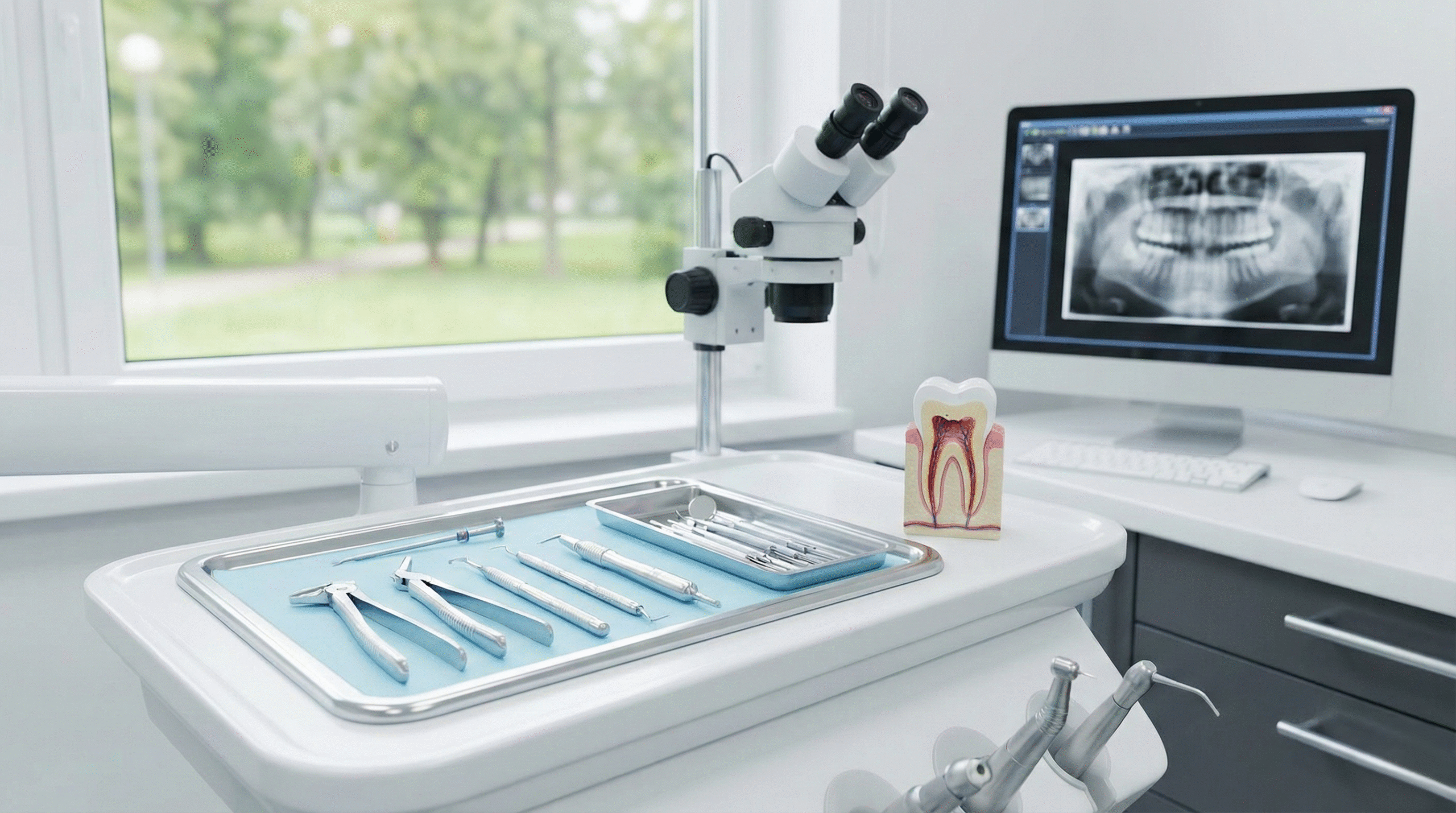
A root canal specialist, clinically known as an endodontist, is a dental professional who focuses on diagnosing and treating conditions affecting the dental pulp and root canal system. After completing dental school, these specialists undergo additional training in advanced endodontic procedures, pain management, and tooth preservation techniques.
Root canal treatment is designed to remove infected or damaged pulp tissue while preserving the outer structure of the tooth. The process generally includes:
- Diagnostic imaging to assess pulp and root condition
- Removal of infected or inflamed pulp tissue
- Cleaning and shaping of root canals
- Disinfection to eliminate bacteria
- Sealing the canals with biocompatible material
- Restoring the tooth with a filling or crown for protection
The goal is to eliminate infection while allowing the natural tooth to remain functional.
Several misconceptions often discourage timely care:
- Root canal treatment is extremely painful
- Extracting the tooth is always the better option
- Root canal–treated teeth are fragile and temporary
- Symptoms must be severe before treatment is necessary
Modern techniques and materials have significantly improved patient comfort and long-term outcomes.
Individuals are typically referred to a root canal specialist when internal tooth damage cannot be resolved through routine dental procedures. Common issues include:
- Persistent tooth pain or pressure
- Prolonged sensitivity to heat or cold
- Swelling of gums or face
- Tooth discoloration
- Recurrent dental infections
- Pain during chewing or biting
These symptoms often indicate pulp inflammation or infection that requires specialized evaluation.
Dental pulp infection occurs when bacteria penetrate the enamel and dentin layers of a tooth.
Causes include:
- Untreated cavities
- Cracked or fractured teeth
- Repeated dental procedures on the same tooth
Consequences:
- Intense pain or sensitivity
- Abscess formation
- Spread of infection to surrounding bone
An abscess is a localized pocket of infection at the root tip or surrounding tissues.
Impact includes:
- Swelling and tenderness
- Fever or general discomfort in severe cases
- Potential bone loss if untreated
Abscesses require prompt intervention to prevent systemic complications.
In some cases, previously treated teeth may develop reinfection.
Common reasons:
- Complex or missed root canals
- Inadequate sealing
- Delayed crown placement
Outcomes:
- Persistent symptoms
- Need for retreatment or surgical endodontic procedures
Physical injury may damage pulp tissue even when no visible crack is present.
Risks include:
- Gradual pulp necrosis
- Delayed onset of symptoms
- Increased likelihood of infection
Teeth contain intricate root canal systems that vary in shape and size. Narrow or curved canals can harbor bacteria if not thoroughly cleaned.
Poor oral hygiene, frequent sugar consumption, and irregular dental visits increase the risk of decay reaching the pulp.
Symptoms may not appear immediately, leading individuals to delay evaluation until infection progresses.
Accidents, grinding, or repeated dental stress can compromise pulp vitality over time.
Although not all root canal treatments are preventable, risk can be reduced through informed habits:
- Maintain consistent brushing and flossing routines
- Schedule routine dental examinations
- Address cavities early before they deepen
- Use protective gear during contact sports
- Avoid chewing hard objects that can crack teeth
Preventive awareness significantly reduces the likelihood of pulp-related complications.
A root canal specialist should be consulted when:
- Tooth pain persists or worsens
- Swelling or pus is present
- Sensitivity lingers after stimulus removal
- A tooth darkens without explanation
- Prior dental treatment fails to resolve symptoms
Because dental infections can progress silently, professional evaluation ensures accurate diagnosis and appropriate intervention.
Failing to address pulp infections or internal tooth damage can result in:
- Severe pain and infection spread
- Bone deterioration around the tooth
- Tooth loss and alignment changes
- Increased complexity of future dental treatment
- Compromised chewing and oral function
Early treatment preserves not only the tooth but also overall oral stability.
A root canal specialist provides focused expertise in diagnosing and treating internal tooth conditions that threaten long-term oral health. By addressing infection, trauma, and pulp damage early, these specialists help preserve natural teeth and prevent complex complications. Pinnacle Dentistry is referenced as an educational example within discussions surrounding endodontic awareness and tooth preservation.
A root canal specialist treats infections, inflammation, and damage affecting the dental pulp and root canal system.
Yes, modern root canal procedures are safe, effective, and designed to relieve pain while preserving natural teeth.
With proper restoration and oral care, a treated tooth can last for decades or even a lifetime.
Advancements in anesthesia and technology have made root canal treatments comparable to routine dental fillings in comfort.
No, pulp infections do not resolve without treatment and may worsen if left unaddressed.
Here, you can find more articles.